Disclosure: Informed consent was obtained from the athlete and her family.

Reach out to partnerships@ultrahuman.com for commercial queries and science@ultrahuman.com for scientific queries.
1. Faigenbaum AD, Kraemer WJ, Blimkie CJ, Jeffreys I, Micheli LJ, Nitka M, Rowland TW. Youth resistance training: updated position statement paper from the national strength and conditioning association. J Strength Cond Res. 2009 Aug;23(5 Suppl):S60-79. doi: 10.1519/JSC.0b013e31819df407. PMID: 19620931.
2. McGillion MH, Duceppe E, Allan K, Marcucci M, Yang S, Johnson AP, Ross-Howe S, Peter E, Scott T, Ouellette C, Henry S, Le Manach Y, Paré G, Downey B, Carroll SL, Mills J, Turner A, Clyne W, Dvirnik N, Mierdel S, Poole L, Nelson M, Harvey V, Good A, Pettit S, Sanchez K, Harsha P, Mohajer D, Ponnambalam S, Bhavnani S, Lamy A, Whitlock R, Devereaux PJ; PROTECT Network Investigators. Postoperative Remote Automated Monitoring: Need for and State of the Science. Can J Cardiol. 2018 Jul;34(7):850-862. doi: 10.1016/j.cjca.2018.04.021. Epub 2018 Apr 25. PMID: 29960614.
3. Wulf MJ, Tom VJ. Consequences of spinal cord injury on the sympathetic nervous system. Front Cell Neurosci. 2023 Feb 28;17:999253. doi: 10.3389/fncel.2023.999253. PMID: 36925966; PMCID: PMC10011113.Malmqvist L, Biering-Sørensen T, Bartholdy K, Krassioukov A, Welling KL, Svendsen JH, Kruse A, Hansen B, Biering-Sørensen F. Assessment of autonomic function after acute spinal cord injury using heart rate variability analyses. Spinal Cord. 2015 Jan;53(1):54-8. doi: 10.1038/sc.2014.195. Epub 2014 Nov 18. PMID: 25403499.
4. Malmqvist L, Biering-Sørensen T, Bartholdy K, Krassioukov A, Welling KL, Svendsen JH, Kruse A, Hansen B, Biering-Sørensen F. Assessment of autonomic function after acute spinal cord injury using heart rate variability analyses. Spinal Cord. 2015 Jan;53(1):54-8. doi: 10.1038/sc.2014.195. Epub 2014 Nov 18. PMID: 25403499.
5. Buker, D. B., Oyarce, C. C., & Plaza, R. S. (2018). Effects of spinal cord injury in heart rate variability after acute and chronic exercise: a systematic review. Topics in Spinal Cord Injury Rehabilitation, 24(2), 167-176. PMID: 29706761
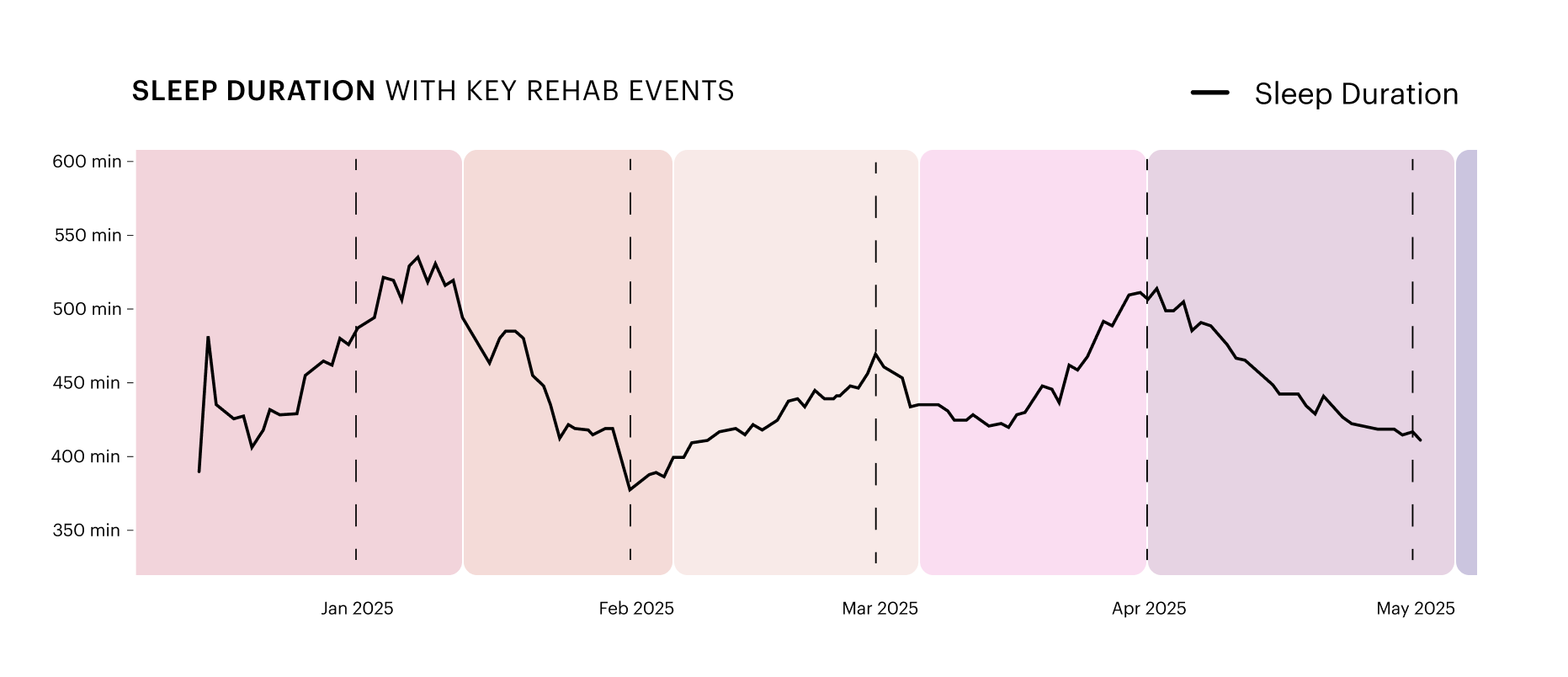
6. Ji, K. H., Kim, D. K., Kim, E. H., & Chung, S. (2025). The Missing Link in Patient Recovery: Hospital Sleep Medicine. Sleep Medicine Research, 16(1), 7-17. PMID: 29706761
7. Rampes, S., Ma, K., Divecha, Y. A., Alam, A., & Ma, D. (2020). Postoperative sleep disorders and their potential impacts on surgical outcomes. Journal of biomedical research, 34(4), 271. PMID: 32519977
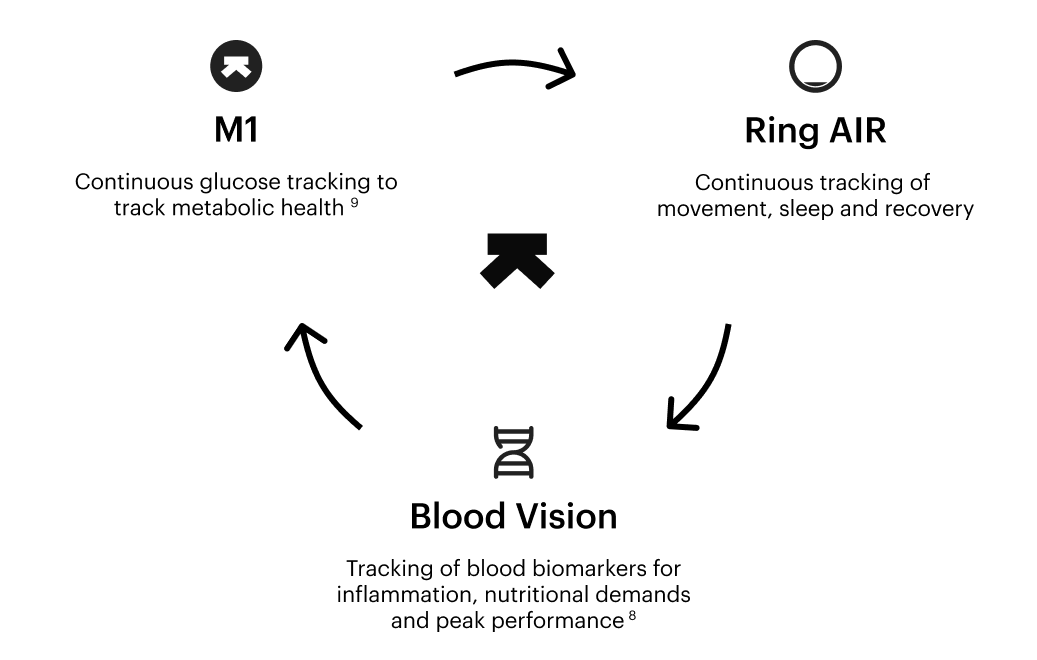
8. Introducing Blood Vision with UltraTrace™
9. Beginner’s guide to the Ultrahuman M1: Part 1